Regi254
Well-Known Member
I'm a bit late (as usual) ..great info! Thank you Sweet Sue. I'm just beginning to read this thread and I will have to reread and study a few words because this is deep and above my knowledge on this side of the cannabis scene. But excited to dig in and learn what I can.What are the pathways into the system and how effective are they?
This is from a white paper at Green House Labs.
So what happens in your body when you take cannabis or cannabinoids?
This primarily depends on which cannabinoids were taken and how they were taken/the route of administration.
Route of administration
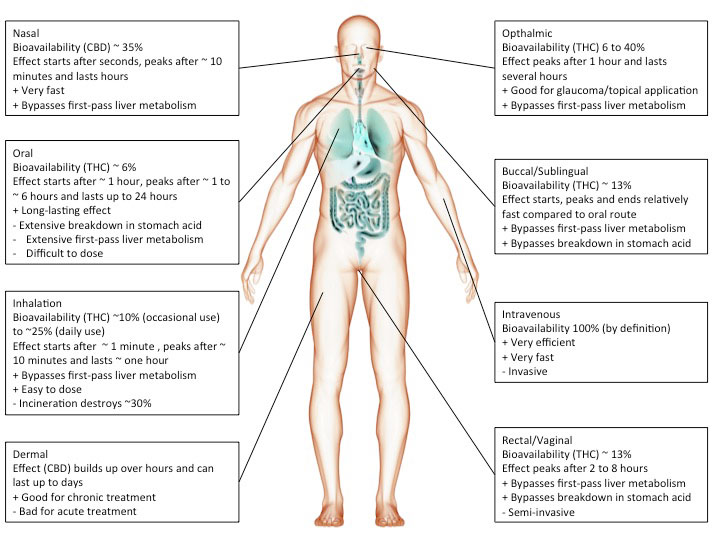
Cannabis or cannabinoids are often smoked but can also be ingested (oil, cake, tea etc.), injected or absorbed through the skin (patch) or mucous membranes (tongue, cheek, rectum). The chosen route of administration has a major impact on the actual effect.
For instance, smoking inevitably heats up cannabinoids causing decarboxylation and a shift from acidic to neutral compounds, which tend to be more biologically active. In addition, the incineration process will render part of the cannabinoids biologically inactive.
However, inhaled cannabinoids enter the bloodstream through the lungs and therefore reach the rest of the body before it passes the liver. This first-pass liver effect can seriously reduce the amount of available cannabinoids. Similarly, ingesting cannabinoids can reduce the amount of available cannabinoids through degradation in the gut/digestive tract.
Heat, chemical degradation or biological degradation/metabolism can dramatically change the amount of cannabinoids that is biologically active: bioavailability. Injected substances are considered 100% bioavailable. Any reduction is ascribed to the route of administration.
Smoked, or inhaled cannabinoids have reported bioavailabilities ranging from 2-56%(Huestis, 2007) with an average of about 30% (McGilveray, 2005). This variability is mainly due to differences in smoking dynamics (how deeply does one inhale, how long does one hold it in). Compared to oral application, the effects of smoking cannabinoids are relatively fast in on- and offset.
Cannabinoids that are absorbed through the mucous membranes in the mouth (buccomucosal application) have bioavailabilities of around 13% (Karschner et al., 2011). Application via the mucous membranes of tongue and cheek or rectal application bypasses degradation in the gut and improves bioavailability.
Distribution
Cannabinoids (and their metabolites/breakdown products) are very lipophilic and are preferentially distributed to fatty tissues such as brain, spleen and body fat rather than aquaeous/water-rich tissues such as blood.
Distribution of THC (other cannabinoids will have similar but not identical distributions based on their respective biochemical properties):
About 1% of biologically available THC reaches the brain.
THC (and metabolites) accumulates in testicular/epididymal fat where it may affect sperm production.
THC crosses the placenta far more efficiently than its metabolites. From 15% (late pregnancy) to 30% (early pregnancy) of maternal plasma THC can be detected in fetal plasma.
THC also accumulates in breast milk (levels 8.4 times higher than plasma). About 10% of maternally consumed THC can be passed on to breast milk.
THC levels peak around 10 minutes after onset of smoking and rapidly go down to ~ 60% of peak after 15 minutes, 20% of peak after 30 minutes and 3% of peak after 2 hours.
THC is degraded to 11-OH-THC, which is also psychoactive, and subsequently to THC-COOH which is not psychoactive. THC-COOH is relatively stabile and can remain detectable for weeks (and is therefore used for drug screening). Most cannabinoid metabolites are excreted with urine (~1/3) or feces (~2/3).
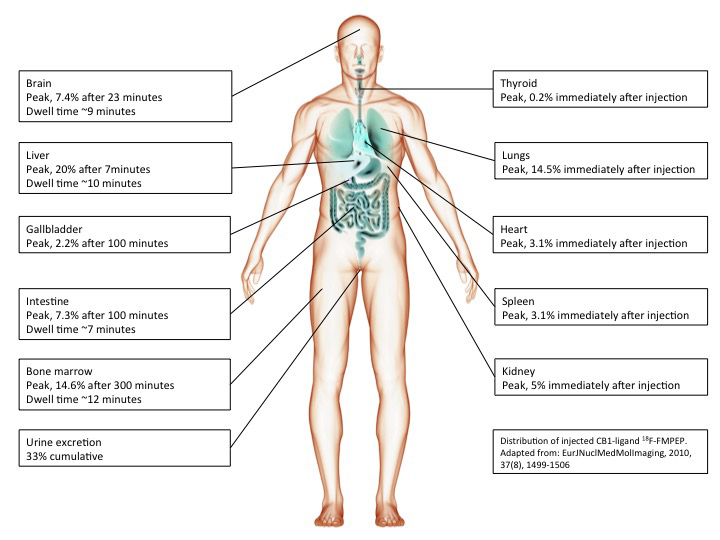
The image below shows the distribution of CB1 receptor ligand 18F-FMPEP after injection into the blood circulation (this distribution can be expected to be similar but not identical to that of THC).
Development
CB1 can be detected in human tissues throughout development (Mato et al., 2003). Comparison of CB1 distribution in the human brain at difference developmental stages shows:
-CB1 expression is relatively low in fetuses, intermediate in children and high in adults.
-CB1 expression in adults is particularly high in hippocampus and basal ganglia.
-CB1 expression in fetuses is particularly high in capsula interna, pyramidal tract and brachium conjunctivum (while not detectable in children and adults) suggesting a transient surge of CB1 in developing neuronal fiber tracts and thus a role in brain development.
Example by numbers
Now let's breakdown what happens when you smoke a cannabis cigarette (adapted from (McGilveray, 2005)).
A cigarette containing 35 mg THC produces peak THC levels of 162 ng/ml plasma 10 minutes after onset of smoking.
An average human has approximately 5l of blood meaning that 162 x 5000 = 810 μg of THC is bioavailable at peak levels, corresponding to bioavailability of 0.81/35 = 2.4% at peak levels.
Peak THC levels are 162 ng/ml. The molecular weight of THC is 314g/mol. 314 ng of THC in 1 ml of plasma corresponds to a 1 μM THC concentration. Therefore, our measured concentration of 162 ng/ml corresponds to 520 nM THC at peak. After 30 minutes, ~20% or ~100 nM is still bioavailable. After 2 hours, ~3% or 15 nM of THC is still bioavailable.
With relative affinities for THC of 10 nM and 24 nM for CB1 and CB2 receptors it can be assumed that most biological activity of THC will have disappeared within 2 hours after smoking a cannabis cigarette (An affinity of 10 nM means that at this concentration 50% of receptors are bound/activated by THC).
Literature
Huestis, M.A. (2007). Human Cannabinoid Pharmacokinetics. Chem. Biodivers. 4, 1770—1804.
Karschner, E.L., Darwin, W.D., Goodwin, R.S., Wright, S., and Huestis, M.A. (2011). Plasma cannabinoid pharmacokinetics following controlled oral delta9-tetrahydrocannabinol and oromucosal cannabis extract administration. Clin. Chem. 57, 66—75.
Mato, S., Del Olmo, E., and Pazos, A. (2003). Ontogenetic development of cannabinoid receptor expression and signal transduction functionality in the human brain. Eur. J. Neurosci. 17, 1747—1754.
McGilveray, I.J. (2005). Pharmacokinetics of cannabinoids. Pain Res. Manag. J. Can. Pain Soc. J. Société Can. Pour Trait. Douleur 10 Suppl A, 15A — 22A.
Full article: Cannabinoids in Your Body
Author: Uncredited
Visuals: Uncredited
Website: GHMedical
Thanks again!



 to cannabis brainstorming central Regi. Glad to have you along. Please don't think you have to read all of that to get to here. This isn't like your normal thread at all. We play a lot here and the posts show it.
to cannabis brainstorming central Regi. Glad to have you along. Please don't think you have to read all of that to get to here. This isn't like your normal thread at all. We play a lot here and the posts show it.  The levity helps break the frustration of prohibition.
The levity helps break the frustration of prohibition. 

 sending some hugs
sending some hugs

 Long time no see, you busy, busy man. Thanks for stopping and letting us know you're still with us. Get some playtime in already.
Long time no see, you busy, busy man. Thanks for stopping and letting us know you're still with us. Get some playtime in already. 