Katelyn Baker
Well-Known Member
Gilles Richard doesn't harbour any illusions about his disease.
It has latched itself to his lungs, his bones and he fears it will eventually seep its way into his brain. Over time, he says, the sickness will prevail.
"I like to say I just want five good years," says Richard, a retired physicist. "But it could be three, it could be two. ... I won't take anything for granted."
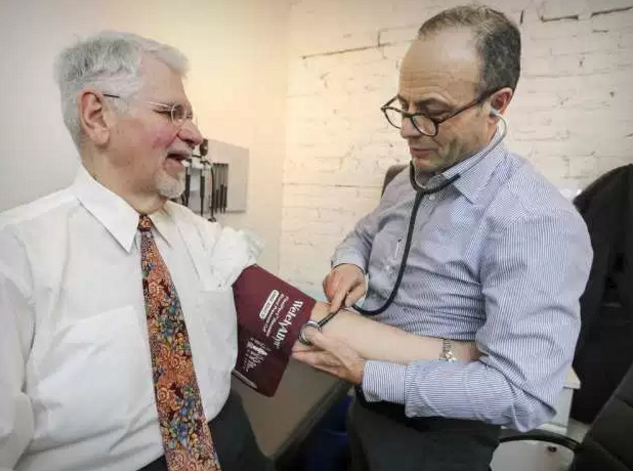
Faced with this grim fate, Richard seems unfazed as he sits in the waiting room of the Santé Cannabis medical clinic on Amherst St. in Montreal's Centre-Sud borough. The 60-year-old wears a suit and tie, he smiles at passersby and offers to chat about topics ranging from molecular biology to the latest episode of The Walking Dead.
Seven years ago, Richard was diagnosed with multi-system sarcoidosis, a rare and incurable genetic disease that causes inflammatory cells to form lumps around vital organs. Richard uses medical cannabis to help manage the chronic pain that's become a fixture in his life.
Because of provincial restrictions surrounding the drug, however, Richard's medical insurance won't cover the cost of cannabis. While marijuana is an increasingly common treatment for chronic pain, epilepsy, multiple sclerosis and dozens of other conditions, the drug exists in a sort of regulatory grey area.
Santé Cannabis is at the centre of an effort to change that.
Next week, the clinic will announce its plan to have Health Canada and the U.S. Food and Drug Administration approve and regulate cannabis-based therapy.
The clinic has partnered with a pharmaceutical research firm to recruit over 500 patients and conduct a one-year study surrounding the safety and efficacy of marijuana in the treatment of chronic pain. A representative of the firm, Tetra Bio-Pharma, says the clinical trial should cost about $2 million and will mostly recruit patients in the Montreal area.
It will be the first such clinical trial in Canadian history.
"With most (drugs) you move slowly, you wait and plan and you're unsure what the testing will reveal," said Dr. Guy Chamberland, Tetra Bio's chief scientific officer. "But I know (cannabis) works, it's just a question of box-checking right now."
The trial's goal is to have North American regulators approve the treatment and issue it a drug identification number – the eight-digit code that indicates a drug can be sold in pharmacies and covered by insurance providers.
Chamberland's firm is working with Algorithme Pharma to test the safety of inhaled-cannabis on 72 human subjects in a study that begins later this winter. The subjects will be paid to smoke marijuana several times a day in a lab where doctors can observe the effects of the drug on their health.
"I don't think we'll have a hard time finding recruits, we'll be paying people to smoke (cannabis)," Chamberland said.
The real challenge begins in the trial's next phase which, according to Chamberland, should begin in about six months. To that end, doctors at Santé Cannabis will recruit and monitor over 500 patients as they use cannabis to treat their chronic pain.
In Quebec, the physician's college only allows doctors to prescribe medicinal cannabis once all other treatment options have been exhausted. The college maintains that there isn't enough research on cannabis to justify approving it.
What this means, in practice, is that by the time a patient is prescribed marijuana, they're often at the end of their rope.
"The people who come to me are desperate, they've run out of options," said Dr. Antonio Vigano, a palliative care doctor at the McGill University Health Centre. "My area of expertise is related to cancer nutrition and rehabilitation. I deal with a lot of people who suffer severe weight loss, loss of appetite, chronic pain and we don't have much that can help them except cannabis."
Vigano, who will oversee the study, works 10 hours a week at Santé Cannabis. On a typical day at the clinic, the waiting room is packed and its receptionist fields up to 200 calls from prospective patients.
Some have degenerative diseases like multiple sclerosis, others suffer from nausea that comes with chemotherapy and others are looking for a solution to the debilitating seizures brought on by epilepsy.
Erin Prosk, the clinic's director, says many of the people who wind up at Sant̩ Cannabis are looking for an alternative to opioids Рa class of painkillers that mimic the effects of heroin. Studies suggest the drug is highly addictive and that an overdose of opioids can be lethal.
Years of opioid use can also lead to significant cognitive delays.
Dr. Michael Dworkind, who also works at the clinic, told the Montreal Gazette that some of his patients reduced their opioid use by using cannabis. He says that because cannabis and opioids target different pain receptors in the brain, there's potential for the drugs to be used in combination.
"This is groundbreaking; the data we gather here can change the way we view chronic pain treatment," said Prosk. "It's also critical that we understand what the risks of cannabis are and monitoring its use for one year will give us a much better idea of that."
With the legalization of recreational marijuana use looming in Canada, Prosk worries that Health Canada's medicinal cannabis program could fall to the wayside.
"There's a medical use for this and one that needs to be recognized by healthcare providers and insurance companies," she said. "To us, this is the first step toward attaining that goal."
Whatever the study's outcome, it's unlikely Richard will benefit from it.
He does a good job hiding his symptoms; he's cheerful, funny and quick to show off pictures of his two grandsons. But Richard clearly struggles: his hands shake, he walks with a cane and he'll spend up to 12 hours in bed each day.
"Some days I have two or three good hours and some days I have none," he says. "I'm still an information junkie, I always have audio books handy or some sort of documentary on the go. Sometimes I prey on people in hospital waiting rooms to see who wants to chat."
"But (the disease) is already affecting my memory and it will probably get worse. I've developed such an incredible tolerance to pain medication. When I went to the surgeon to have a (lump) removed from my arm, what they were shooting me up with had no effect. Whether it's opioids or cannabis, this is what my body needs until I finish my life."
News Moderator: Katelyn Baker 420 MAGAZINE ®
Full Article: Montreal Doctors Spearhead Cannabis Clinical Trial
Author: Christopher Curtis
Contact: 1-514-987-2222
Photo Credit: None Found
Website: Montreal Gazette
It has latched itself to his lungs, his bones and he fears it will eventually seep its way into his brain. Over time, he says, the sickness will prevail.
"I like to say I just want five good years," says Richard, a retired physicist. "But it could be three, it could be two. ... I won't take anything for granted."
Faced with this grim fate, Richard seems unfazed as he sits in the waiting room of the Santé Cannabis medical clinic on Amherst St. in Montreal's Centre-Sud borough. The 60-year-old wears a suit and tie, he smiles at passersby and offers to chat about topics ranging from molecular biology to the latest episode of The Walking Dead.
Seven years ago, Richard was diagnosed with multi-system sarcoidosis, a rare and incurable genetic disease that causes inflammatory cells to form lumps around vital organs. Richard uses medical cannabis to help manage the chronic pain that's become a fixture in his life.
Because of provincial restrictions surrounding the drug, however, Richard's medical insurance won't cover the cost of cannabis. While marijuana is an increasingly common treatment for chronic pain, epilepsy, multiple sclerosis and dozens of other conditions, the drug exists in a sort of regulatory grey area.
Santé Cannabis is at the centre of an effort to change that.
Next week, the clinic will announce its plan to have Health Canada and the U.S. Food and Drug Administration approve and regulate cannabis-based therapy.
The clinic has partnered with a pharmaceutical research firm to recruit over 500 patients and conduct a one-year study surrounding the safety and efficacy of marijuana in the treatment of chronic pain. A representative of the firm, Tetra Bio-Pharma, says the clinical trial should cost about $2 million and will mostly recruit patients in the Montreal area.
It will be the first such clinical trial in Canadian history.
"With most (drugs) you move slowly, you wait and plan and you're unsure what the testing will reveal," said Dr. Guy Chamberland, Tetra Bio's chief scientific officer. "But I know (cannabis) works, it's just a question of box-checking right now."
The trial's goal is to have North American regulators approve the treatment and issue it a drug identification number – the eight-digit code that indicates a drug can be sold in pharmacies and covered by insurance providers.
Chamberland's firm is working with Algorithme Pharma to test the safety of inhaled-cannabis on 72 human subjects in a study that begins later this winter. The subjects will be paid to smoke marijuana several times a day in a lab where doctors can observe the effects of the drug on their health.
"I don't think we'll have a hard time finding recruits, we'll be paying people to smoke (cannabis)," Chamberland said.
The real challenge begins in the trial's next phase which, according to Chamberland, should begin in about six months. To that end, doctors at Santé Cannabis will recruit and monitor over 500 patients as they use cannabis to treat their chronic pain.
In Quebec, the physician's college only allows doctors to prescribe medicinal cannabis once all other treatment options have been exhausted. The college maintains that there isn't enough research on cannabis to justify approving it.
What this means, in practice, is that by the time a patient is prescribed marijuana, they're often at the end of their rope.
"The people who come to me are desperate, they've run out of options," said Dr. Antonio Vigano, a palliative care doctor at the McGill University Health Centre. "My area of expertise is related to cancer nutrition and rehabilitation. I deal with a lot of people who suffer severe weight loss, loss of appetite, chronic pain and we don't have much that can help them except cannabis."
Vigano, who will oversee the study, works 10 hours a week at Santé Cannabis. On a typical day at the clinic, the waiting room is packed and its receptionist fields up to 200 calls from prospective patients.
Some have degenerative diseases like multiple sclerosis, others suffer from nausea that comes with chemotherapy and others are looking for a solution to the debilitating seizures brought on by epilepsy.
Erin Prosk, the clinic's director, says many of the people who wind up at Sant̩ Cannabis are looking for an alternative to opioids Рa class of painkillers that mimic the effects of heroin. Studies suggest the drug is highly addictive and that an overdose of opioids can be lethal.
Years of opioid use can also lead to significant cognitive delays.
Dr. Michael Dworkind, who also works at the clinic, told the Montreal Gazette that some of his patients reduced their opioid use by using cannabis. He says that because cannabis and opioids target different pain receptors in the brain, there's potential for the drugs to be used in combination.
"This is groundbreaking; the data we gather here can change the way we view chronic pain treatment," said Prosk. "It's also critical that we understand what the risks of cannabis are and monitoring its use for one year will give us a much better idea of that."
With the legalization of recreational marijuana use looming in Canada, Prosk worries that Health Canada's medicinal cannabis program could fall to the wayside.
"There's a medical use for this and one that needs to be recognized by healthcare providers and insurance companies," she said. "To us, this is the first step toward attaining that goal."
Whatever the study's outcome, it's unlikely Richard will benefit from it.
He does a good job hiding his symptoms; he's cheerful, funny and quick to show off pictures of his two grandsons. But Richard clearly struggles: his hands shake, he walks with a cane and he'll spend up to 12 hours in bed each day.
"Some days I have two or three good hours and some days I have none," he says. "I'm still an information junkie, I always have audio books handy or some sort of documentary on the go. Sometimes I prey on people in hospital waiting rooms to see who wants to chat."
"But (the disease) is already affecting my memory and it will probably get worse. I've developed such an incredible tolerance to pain medication. When I went to the surgeon to have a (lump) removed from my arm, what they were shooting me up with had no effect. Whether it's opioids or cannabis, this is what my body needs until I finish my life."
News Moderator: Katelyn Baker 420 MAGAZINE ®
Full Article: Montreal Doctors Spearhead Cannabis Clinical Trial
Author: Christopher Curtis
Contact: 1-514-987-2222
Photo Credit: None Found
Website: Montreal Gazette


